Navigating MCAS: Is a Low Histamine Diet the Right Step?
If you’ve been diagnosed with Mast Cell Activation Syndrome (MCAS), or suspect you’re dealing with it, chances are you’ve come across information about the Low Histamine Diet on Google, MCAS Facebook groups or blogs. It’s one of the most common areas people reach out to us for support with.
While a low histamine diet can help helpful for some, it also comes with some important caveats, and potential pitfalls. Before diving into this elimination diet, it's worth understanding how (and if) this approach fits into your MCAS management journey.
What is Mast Cell Activation Syndrome (MCAS)?
Mast Cell Activation Syndrome (MCAS) occurs when our mast cells, a white blood cell that lives in our connective tissue, releases chemical mediators too readily.
In people without MCAS, our mast cells serve as a key defence mechanism that release histamine, heparin and inflammatory cytokines in response to potential threats. These chemicals cause inflammation, which helps to draw a wider immune response to the area to assess and manage said threats.
In people with MCAS, excessive mast cell activation results in chronic inflammation and symptoms. Given that connective tissue is present throughout the entire body, symptoms can occur in any organ system, and can present very differently person-to-person.
What is Histamine Intolerance? Why can if affect people with MCAS?
Histamine intolerance occurs when the amount of histamine in our system exceeds our body's capacity to break it down, resulting in sensitivities to certain foods. It can occur in people with and without MCAS.
Foods that people commonly react to with histamine intolerance can include: leftovers, fermented food (e.g. sauerkraut, yoghurt, wine), aged food (e.g. aged meats and cheeses), tomatoes, chocolate, bananas, peanuts, shellfish, avocadoes, strawberries, canned foods (e.g. sardines), vinegar-based products, bone broth and more.
Everyone has a histamine threshold - or the amount of histamine their body can handle on any one day, hour or minute. The 'Histamine Bucket' analogy is often used here, describing how symptoms arise when our histamine bucket is too full and 'overflows'. Food is a common element that can contribute to filling up our histamine bucket, as histamine is an amino acid which is commonly present in food, as well as something that is produced by protein breakdown over time.
In this context, it makes sense that cutting down on what is filling up our Histamine Bucket (e.g. high histamine foods) by implementing a Low Histamine Diet would help.
However, in MCAS I believe that simply implementing a Low Histamine Diet often leads to missing the 'bigger picture' of factors that could be addressed, and in many cases can be harmful to clients.
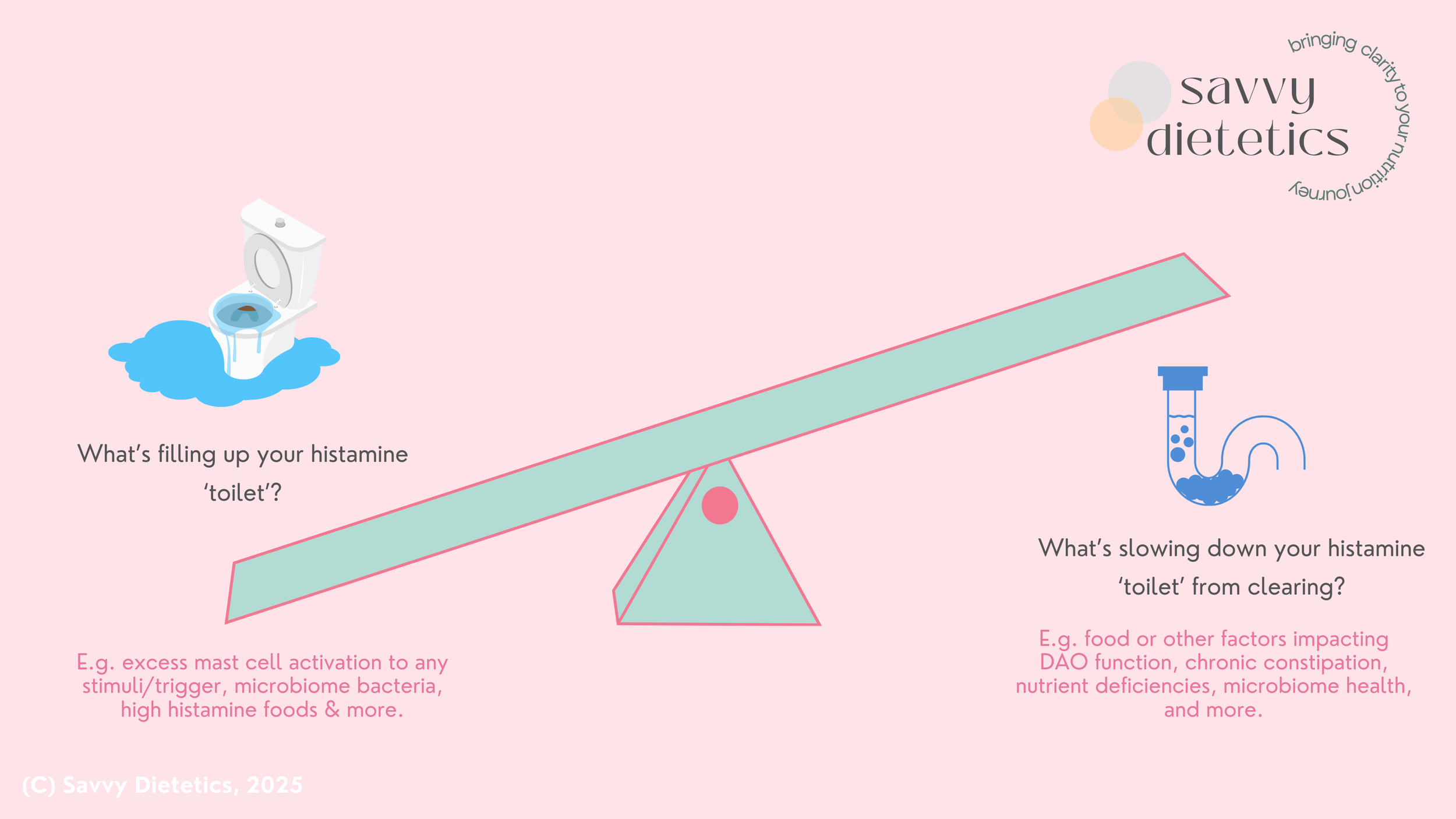
Our 'Histamine Toilet' Analogy - don't forget to optimise histamine degradation
One major aspect which 'Histamine Bucket' theory neglects is that for many people with MCAS, our ability to break down histamine is often impaired.
Because of this, I prefer to use the analogy of a 'Histamine Toilet' - as with a toilet, overflowing water can be caused by both too much waste going into the toilet (e.g. too much histamine from food, excess mast cell activation and more), and a blockage in the pipes (e.g. factors which impede histamine clearance).
Re-thinking the ‘Histamine Bucket’ as a ‘Histamine Toilet’
How does our body detoxify histamine?
DAO Enzyme
Diamine Oxidase (DAO) is one of the key enzymes in our body that breaks down histamine. It's largely produced in our small intestine, where it interacts with the histamine in our food to assist with digesting and clearing it.
When there is low grade (or significant) inflammation in our small intestine, DAO production and function can be significantly affected. Excess cortisol and adrenaline (common in chronic stress or hyperadrenergic Postural Orthostatic Tachycardia Syndrome) can also down regulate DAO activity. This can lead to histamine entering our blood stream more easily, causing gastrointestinal and systemic symptoms.
HNMT Enzyme and Phase 2 Liver Detoxification
Histamine N-methyltransferase (HNMT) is an enzyme present throughout the body (especially liver and kidneys) which breaks down histamine by adding a methyl group. Poor methylation due to genetic polymorphisms, micronutrient deficiencies (e.g. folate and B12) and excess estrogen (e.g. in PCOS where testosterone is aromatised to estrogen in adipose tissue, or endometriosis where lesions secrete estrogen) something we see commonly in our MCAS clients, which further impacts histamine breakdown.
In the liver, this is referred to as the 'Methylation' pathways, which occurs in Phase 2 detoxification. Other Phase 2 liver pathways which are involved in histamine breakdown include Sulfonation (impacted by low methionine, B6 and B12, and cytokines downregulating enzyme activity), Glucuronidation (impacted by exposure to environmental toxins and low Vitamin C) and Acetylation (impacted by poor fat digestion and Vitamin B5 deficiency).
Histamine and Our Gut Microbiome
One of my favourite papers is Histamine Intolerance Originates in the Gut. While this title as a statement is not quite true for people with MCAS (as mast cells secreting histamine can contribute to exceeding our histamine threshold), it does allow us to appreciate just how much our microbiome can influence histamine production, sensitivity and detoxification.
Microbiome bacteria hold a fascinating role when it comes to regulating our histamine threshold. There is still so much that research is yet to uncover, but a few key favourite facts of mine include:
Many bacteria break down histamine (e.g. Lactobacillus Rhamnosus and Bifidobacerium Longum). These bacteria are often deficient in unhealthy microbiomes.
Many bacteria secrete histamine, or can directly activate mast cells (e.g. various Clostridium and Enterococcus species). These are often opportunistic and take advantage of unhealthy microbiomes.
Some bacteria secrete an inflammatory chemical called Lipopolysaccharide (LPS) which can increase our reactivity to the histamine which is currently in our gut, by a few mechanisms including increasing the number of H1 histamine receptors on mast cells (making our mast cells more likely to over-activate) and H2 receptors (influencing gastrointestinal symptoms).
This is why managing chronic constipation, and using foods or prebiotics and probiotics (in a targeted way) can be incredibly helpful for some people with MCAS.
The Pitfalls of Low Histamine Diets and Dietary Elimination
For most people that we work with at Savvy Dietetics, a strict Low Histamine Diet is not physically or financially accessible, and can pose a significant threat to physical and mental health (including relationship with food).
Aspects to consider when thinking about undertaking a Low Histamine Diet include:
Cost - is often higher than most people's standard diet, as fresh, high quality protein is required (butcher bought preferred).
Food preparation - in strict Low Histamine Diets, food often needs to be prepared fresh daily (or bulk prepared and frozen), which carries a significant burden with cooking and cleaning.
Neurodivergence - strict Low Histamine Diets often involve eliminating safe foods. This can lead to people who have strong sensory preferences skipping meals, or eating less, which is a significant risk factor for malnutrition.
Social and emotional health - strict elimination diets can mean that eating out can become logistically tricky, which we see can often impact people's social life and emotional health.
Malnutrition - all strict elimination diets are a risk factor for undereating and malnutrition, especially in individuals who also have Hypermobility (e.g. EDS or HSD) or other Invisible Illnesses (POTS, ME/CFS, autoimmunity). Under eating is also a threat to our body, which we suspect increases mast cell activation.
Microbiome - limiting fibre rich foods (many of which are reduced on a Low Histamine Diet) can adversely impact microbiome health. This is important considering that low microbiome diversity can lead to opportunistic species growing which produce more histamine and directly activate mast cells. Many of the 'good' bacteria species which are present in healthy microbiomes help in breaking down histamine.
Nutrient deficiencies - restricting vitamin and mineral rich foods is a significant risk for developing micronutrient deficiencies. Micronutrient deficiencies such as low Vitamin C, Vitamin D, Zinc and Copper can worsen histamine intolerance in MCAS by slowing reactions which break down histamine (as micronutrients are co-factors in these reactions) and worsening immune dysregulation.
Relationship with food - due to a combination of the above, relationship with food is often impacted by strict elimination diets, especially when they are undertaken for a prolonged period without an 'exit plan'. This is a risk factor for developing disordered eating behaviors, or an eating disorder.
At Savvy Dietetics, we work with many clients who have MCAS and find that we can often get good results and symptom relief without strict dietary histamine elimination. For times when we think a more strict Low Histamine Diet is needed, we provide thorough planning sessions, support, and an exit plan, and aim to only significant restrict diet for a maximum of 8 weeks.
How can I sustainably use Nutrition & Dietetic strategies to manage MCAS?
Nutrition can be a powerful part of your MCAS management toolkit, however finding a set of strategies that are effective and sustainable for you requires an individualised approach.
At Savvy Dietetics, areas that we may address to assist in MCAS management may include: microbiome health, optimising micronutrient intake, blood sugar regulation, gentle dietary histamine alterations (only when safe), evidence-based nutraceuticals, dysautonomia management and much more.
If you have any questions, or if you are seeking support with MCAS, Hypermobility or complex gastrointestinal concerns, please don't hesitate to reach out.
~ Savvy
Savvy Dietetics is an Australian Nutrition & Dietetics clinic passionate about helping people with invisible illness and complex gastrointestinal concerns, including Hypermobillity & Co. Consult information and bookings can be found here, and if you have any specific questions, feel free to email us at admin@savvydietetics.com.au.
This blog was published on 26th August 2025 and received 550 views before we migrated website platforms in January 2026.