Chronic constipation in hypermobility: a dietitan's guide
For many hypermobile people, dealing with strained, incomplete and irregular bowel motions have been a fact of life since early age.
What's the go?
Research suggests that many people who have EDS or hypermobility struggle with constipation, with 38.5% meeting criteria for chronic constipation in one paper (Nelson, 2015 - 687 patients with varying types of EDS) and 45.4% in another (Alomari, 2020 - 218 patients with hEDS).
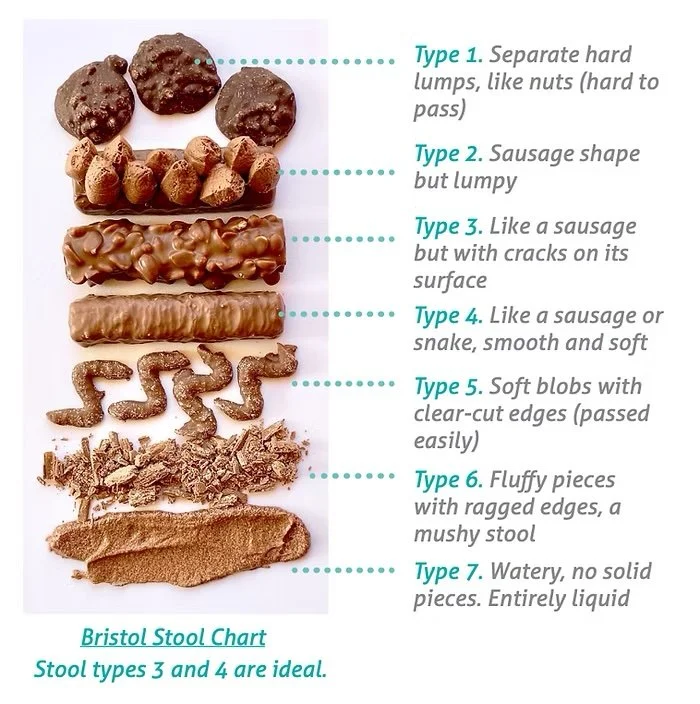
While definitions of constipation vary, a generally accepted one is passing less than three bowel motions per week, and/or struggling with passing these due to straining or other factors. To be chronic, an individual has to experience this for more than three months.
Source: Dietitian Connection
Chronic constipation can have a big impact on quality of life - from feeling uncomfortable and bloated, and the body dysmorphia this can bring, to the burden of having to remember laxatives and dreading going to the toilet.
At the most extreme end of chronic constipation in hypermobility, a person can have little to know bowel motions without additional help (laxatives, enemas, etc) and be at high risk of fecal loading and impacted fecal matter.
Fecal impaction, or ileus, refers to a buildup or stool in the large (sometimes small) intestine. If left untreated this form of intestinal obstruction can sometimes lead to serious complications including stretching or perforation of the intestinal wall, or twist the colon, leading to a lack of blood and tissue death.
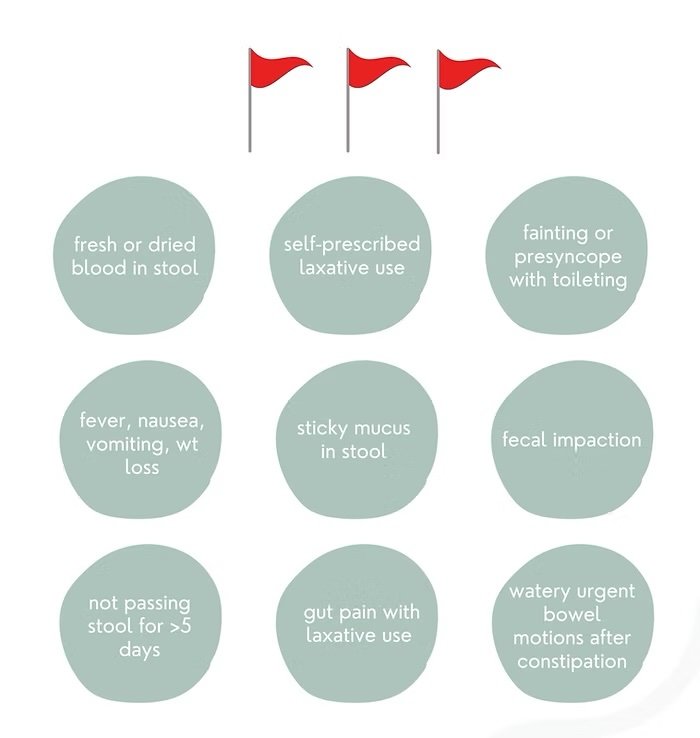
Red flags
Before we start, let's cover some 'red flags' for constipation that would warrant more urgent further investigation by a GP, Gastroenterologist or Dietitian:
Source: @hypermobility.dietitian
Depending on your symptoms, your medical team may organise a variety of tests for you. These can range from:
fecal tests (e.g. to detect inflammation via calprotectin, pancreatic function, or active parasites)
abdominal x-ray (to assess level of fecal loading)
endoscopy (upper gastrointestinal camera scope)
colonoscopy (lower gastrointestinal camera scope)
blood tests
and more
Your medical team can also prescribe medications which can help, like laxatives or prokinetics (help gut move faster). They can also review medication your are currently on which to identify ones that cause slow gut motility (e.g. anti-nausea medication ondansetron). Lastly, their input helps to inform our work as dietitians to safely help you.
Why can hypermobile people experience constipation?
There are SO many reasons hypermobile people can be constipated. And from my clinical experience, in most cases there are multiple reasons, not just one.
Here is a brain dump of some of the contributing factors to slow, strained stools. This is not a complete list, so check in with your health team!
Hypermobile connective tissue
Stretchy colon tissue - the colon can struggle to contract, and propel stool through the intestines. Over time, if left untreated this can worsen, stretching this tissue further
Tight pelvic floor - hypermobile people often stabilise our body using the pelvic floor, and too much tightness here can make toileting difficult
Rectal or genital prolapse - again, common in hypermobility, and can impact movement of stool through the intestines
Vascular compression syndromes (e.g. MALS, SMA, nutcracker) - slipping ligaments can reduce blood flow or change nervous regulation to certain areas of the gut, slowing motility
Autonomic nervous system (dysautonomia)
Low innervation to the intestines from sympathetic overdrive (being in flight-flight mode) - sometimes dysautonomias can inhibit peristalsis (wave like contractions that move food through the gut), worsening or causing constipation
Dehydration from low fluid intake or increased urine output (e.g. POTS)
Gut, microbiome & diet
Low soluble fibre - not enough sticky gooey fibre can make it hard to move the bowel motion through the gut
Excess dietary fibre - although this is less common, having too much fibre (especially in the forms of fibre powders and supplements!) can worsen fecal loading and constipation in hypermobile people.
Not eating enough, or at regular times - both can trigger constipation!
SIBO & methane - overgrowth of certain bacteria in the small intestine and/or methane producing archaea slow gut motility
Poor bile flow - bile is our body's natural laxative! Slow bile flow from a variety of factors can contribute to constipation
Low gut serotonin - serotonin is a key regulator of gut motility, and mostly produced by the bacteria in our gut microbiome (although serotonin from our gut bugs can't enter the brain!). Changes in gut flora may mean not enough serotonin is produced, which seems to worsen constipation
Cow's milk protein sensitivity/allergy and coeliac disease - these can manifest as constipation
Low magnesium - while magnesium supplements can be an osmotic laxative if we take too much (excess magnesium drags water into bowels), it's key for regulating muscle contraction & release. If intake/levels are suboptimal, increasing magnesium can help smooth muscle in our gut work better (peristalsis)
Other gut microbiome changes can impact motility too
Neurodivergence
Reduced interoception - struggling to understand bathroom cues can contribute to constipation
Struggling to maintain regular eating times and patterns
Other
Endometriosis adhesions - impacting the pelvic floor and intestine structure
Mirena IUD - progesterone can slow gut motility in some
Low physical activity - movement, even gentle, helps move food through the intestines
Malnutrition - smooth muscle loss in the small intestine can worsen motility
Medications, including opioids (strong painkillers), ondansetron (specific anti-nausea medication) and many more can cause constipation, so chat to your GP or pharmacist!
Supplements like iron, specific probiotics and more can cause constipation
So, what should I do?
If you tick any boxes in the red flag section above, I'd urge you to:
If you think you have a fecal impaction, see your GP urgently or go to Emergency if you have a fever, abdominal pain, nausea or vomiting
If not displaying high risk symptoms:
Chat to your GP
Seek a referral to a Gastroenterologist, if appropriate
Book in to see a gut health Dietitian
Consider seeing a Pelvic Floor Physiotherapist
As a Dietitian, we'll be able to help with the practicalities of nutrition and supplements. This can include strategies to tolerate more soluble fibre, considering supplements if appropriate (e.g. prebiotics, laxatives, magnesium), optimising hydration, investigating food intolerances and referring on for further help when needed.
Starting with the basics, here are some areas that are often safe to work on:
Hydration - if you're not drinking enough water, start here.
Sticky, gooey soluble fibres - if tolerated, foods like chia seeds, psyllium, oats and lentils all can help to bulk and soften the stool. Start low and go slow here, and make sure to pair with water otherwise constipation can worsen. In Australia the fibre recommendation is 25-30g per day - check with your dietitian if unsure as you may need more/less than this, or to prioritise certain types of fibre. Note: for people with fecal impaction or very significant fecal loading, you may need to reduce dietary fibre intake and cease fibre-containing supplements - chat to your health team.
Nervous system regulation - any strategies that calm the nervous system have potential to help. Some of my clients love the guided hypnotherapy app Nerva, others like to do their own meditations or mindfulness moments, or work with a provider who can help here.
Warm compress & massage - a heat pack against the belly, and gentle massage if pain-free can also help in some cases. The UK's National Health Service has a wonderful 'Self-abdominal massage handout' available through search engines.
Gentle movement - if safe, gentle movement can sometimes stimulate gut motility,
Medical treatments for constipation
Depending on your medical conditions and why you are constipated, your doctor may also (but not always) prescribe one or a range of the following medications:
Laxatives
Osmotic laxatives draw water into the bowel motion, e.g. lactulose, Osmolax, PEG
Fibre/bulking laxatives bring sticky gooey fibre into the bowel, which can help stimulate a motion e.g. Phloe, PHGG, psyllium
Stimulant laxatives activate gut smooth muscles, triggering a motion, e.g. Ducolax, senna
Suppositories are inserted rectally to produce a bowel motion
Prokinetic medications
Domperidone is an anti-nausea drug that also increases motility in the stomach and intestines
Prucalopride increases peristalsis by acting on serotonin receptors, often not used as a first-line strategy
Enemas - insertion of water/solution into the rectum to stimulate a bowel motion
Do not trial any of these without medical (GP or specialist) supervision!
As always, reach out or book a discovery call online if you're interested in troubleshooting lifestyle strategies for chronic constipation & hypermobility.
Savita
@hypermobility.dietitian
This blog post was originally published on 7th November 2023 and received 2,825 views before we migrated websites in January 2026.