Median Arcuate Ligament Syndrome (MALS): A Hypermobile Dietitian's Guide
Over the past few years, we've seen a growing number of hypermobile clients presenting with abdominal vascular compressions, including Median Arcuate Ligament Syndrome (MALS) - also called coeliac artery compression syndrome.
In this blog post, we'll walk through what MALS is, answer some of the most common questions we hear in clinic, and hopefully offer some clarity in a way that’s straightforward and easy to digest.
If you're exploring vascular compression syndromes, you may be interested in our related post, Superior Mesenteric Artery Syndrome: A Hypermobile Dietitian's Guide.
What is Median Arcuate Ligament Syndrome (MALS)?
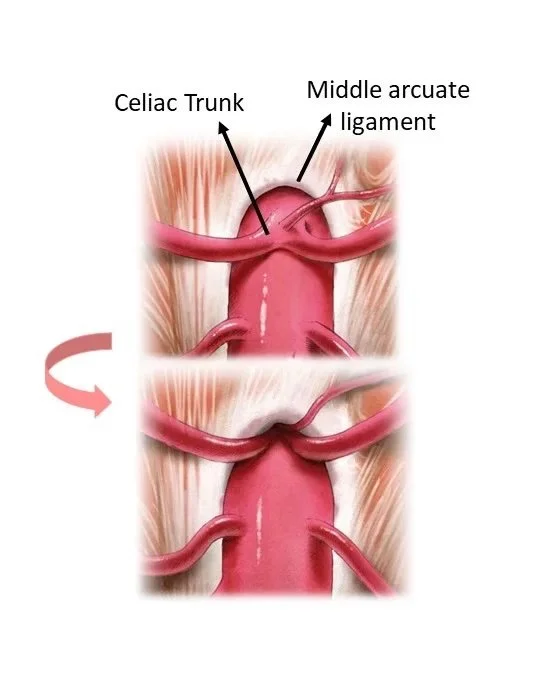
Credit: https://www.aescov.es/en-US/sindromes-compresivos-vasculares/ligamento-arcuato-medio/
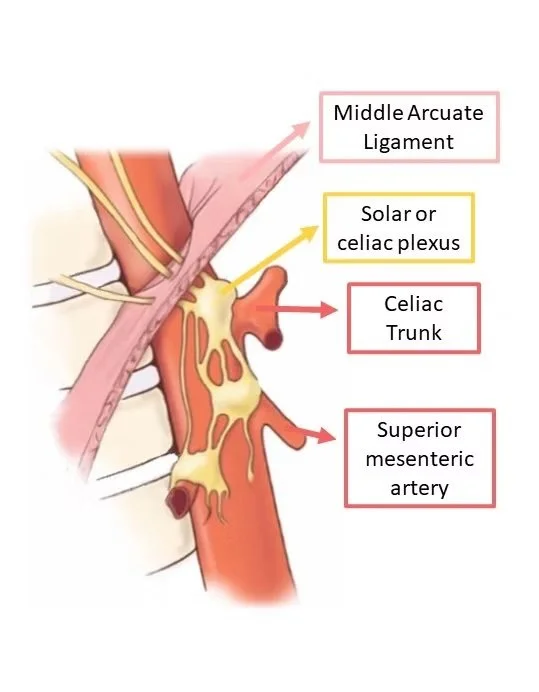
Median Arcuate Ligament Syndrome occurs when the median arcuate ligament droops too low, and presses on the coeliac artery ('vascular MALS'), coeliac nerve plexus ('neurogenic MALS') or both.
Our median arcuate ligament is an arch-shaped piece of fibrous connective tissue that connects the two cura of the thoracic diaphragm (the points that anchor our breathing diaphragm to our spine). Because of its arch shape, the median arcuate ligament also forms part of the 'aortic hiatus', or the circle shaped gap that our aorta (big, tree trunk like blood vessel) goes through.
Vascular MALS - compression of the coeliac artery
When the coeliac artery is compressed, blood flow through this vessel can become reduced or turbulent.
Since the coeliac artery supplies blood to key upper gastrointestinal organs (including the stomach, liver, oesophagus, small intestine, gall bladder), impaired flow can lead to generalised upper abdominal pain and compromised organ function, driven by transient ischaemia (temporary lack of blood supply, and the oxygen and nutrients that blood delivers).
Over time, this may lead to structural changes in the artery such as stenosis (narrowing) at the site of compression, and dilation (widening) after or sometimes before the site of compression due to altered blood flow dynamics.
There are also several factors that can contribute to the fluctuating nature of vascular MALS. First, the degree of coeliac artery compression can vary throughout the breathing cycle (inhale - neutral breath - exhale). In many cases, the artery is most significantly compressed during exhalation, when the diaphragm moves upward and applies pressure to the vessel. Second, many of the upper gastrointestinal organs supplied by the coeliac artery also receive blood from other arteries through collateral circulation. This overlapping blood supply may help maintain perfusion at times, contributing to the intermittent nature of symptoms seen in some people.
Neurogenic MALS - compression of the coeliac nerve plexus
Compression of the coeliac plexus (a dense bundle of sympathetic nerves near the origin of the coeliac artery) can lead to chronic nerve irritation and overstimulation of the sympathetic nervous system - our 'fight-flight-freeze' response.
The coeliac plexus provides sympathetic innervation to many upper gastrointestinal organs, including the stomach, liver, pancreas, gallbladder, and portions of the small intestine. While the sympathetic nervous system plays a key role in regulating heart rate and blood pressure, it also affects gastrointestinal function - particularly motility, digestive juice (stomach, bile and exocrine pancreatic) secretion, and blood flow to digestive organs.
Because this plexus only delivers sympathetic input (without balancing parasympathetic 'rest-digest' signals), its chronic activation due to compression can result in a persistent stress-like state in the body and gut, alongside nerve-related pain.
Compression of the coeliac plexus may also mimic or worsen symptoms of dysautonomia, particularly Postural Orthostatic Tachycardia Syndrome (POTS). This is a key clinical consideration, especially as hypermobility syndromes like Ehlers-Danlos Syndrome are frequently associated with both POTS and MALS.
Why can MALS develop in Hypermobility conditions (e.g. HSD, hEDS)?
Emerging research points to the role of altered connective tissue structure in the form of collagen laxity as a likely contributing factor for MALS development in people with Hypermobility conditions such as Hypermobility Spectrum Disorder (HSD) and hypermobile Ehlers-Danlos Syndrome (hEDS).
In individuals with Hypermobility conditions, it’s thought that this increased tissue laxity may allow the median arcuate ligament to sit lower than usual, particularly when upright. This compression can be further exacerbated by the effects of gravity, postural changes, and common co-existing conditions such as visceroptosis (sagging of abdominal organs) and gastroptosis (downward displacement of the stomach).
More research is needed to fully understand the relationship between hypermobility and vascular compression syndromes.
How is MALS diagnosed?
There are a few investigations that can be used to identify and diagnose Median Arcuate Ligament Syndrome.
Options can include:
Doppler Ultrasound
This is the most common and accessible options we see our Australian clients referred to, and they work by visualising blood flow and the vascular system. Usually, measurements of the blood vessel structure and flow rate are recorded in a variety of postures (lying down, standing up, and often propped up at a 45oc angle or sitting) and across both the inhale, exhale and neutral breath, given that all of these factors can impact anatomy and MALS compression.
Note that for some clients who only have neurogenic MALS, doppler ultrasounds may miss this diagnosis given that there may not always be an element of vascular compression.
CT Angiogram
This procedure involves contrast being delivered into the vascular system, and a series of images being taken via x-ray to visualise the coeliac artery and nearby structures. The technician will usually require you to hold an exhale breath, to fully capture the extent of any potential MALS here.
Positive response to a coeliac plexus nerve block
This is an emerging method that may be helpful in diagnosing neurogenic MALS - more information below.
Other imaging techniques such as Magnetic Resonance Angiogram may be used if the above are inconclusive.
It's important to note that these generally require experienced practitioner to perform and/or interpret these tests. We have seen many cases of MALS being initially dismissed until a more knowledgeable practitioner reviewed the results, redid the test themselves, or ordered the test at a facility which uses more advanced protocols.
Symptoms of MALS
Symptoms associated with MALS vary significantly, but may include:
Upper abdominal pain, especially immediately after food or liquid intake. Pain or discomfort may radiate through to the back of the sternum. This can be a result of reduced blood flow to these areas, or nerve compression.
Relief in symptoms when leaning forwards
Exacerbation in pain or symptoms during exhalation, when the diaphragm rises
Significant dysautonomia (e.g. Postural Orthostatic Tachycardia Syndrome, Orthostatic Hypotension) which is difficult to manage with usual treatment (sodium, fluid, medications)
Breathing issues and thoracic diaphragm pain
Food avoidance, anxiety around food, malnutrition and unintentional weight loss
This may present as eating disorder-like behaviors, especially in neurodivergent clients. However, our experience is that in this population, most disordered eating is usually secondary to MALS symptoms.
Gastroparesis, or slow stomach emptying
Persistent nausea
Vomiting, reflux and regurgitation
Upper abdominal bloating
It is important to note that these symptoms can overlap with many other presentations and gastrointestinal disorders. In many cases, MALS-like symptoms may not be MALS. Saying that, if your symptoms are persistent and impact your nutrition, it may be worth discussing MALS investigations with your medical team.
How severe is MALS?
The impact that MALS has can vary significantly person-to-person.
Many of the clients we work with have transient symptoms which ebb and flow, for instance flaring up with episodes of increased mast cell activation syndrome (which markedly increase visceral hypersensitivity, and may alter connective tissue quality) or general stress (which may result in a POTS flare and more fecal loading). In these clients, putting together a 'toolkit' of strategies to manage pain and nutritional status (malnutrition) are key priorities.
Other clients may find that symptoms are more persistent and impactful, especially when MALS results in ongoing low food and fluid tolerance - which are both key risk factors for developing malnutrition. If thorough conservative management has not yet been explored, some of these clients may be able to gain enough improvement through these therapies alone, however some clients may need to explore interventional approaches.
Conservative MALS Management
Conservative management of MALS often involves a multidisciplinary approach (allied health and medical care), focussing on strategies that may directly or indirectly work to manage symptoms and reduce the severity of compression. Most clients that we work with at Savvy Dietetics are able to manage their MALS conservatively.
Non-Dietetic Management
Although many symptoms associated with MALS are gastrointestinal and can significantly impact nutrition, I cannot estimate how valuable non-Dietetic input is for the successful conservative management of MALS - especially physical therapy.
Given that MALS is largely a structural issue, it makes sense that physical therapy could have the potential to reduce or manage MALS. Anecdotally, our MALS clients who have made the most significant improvement in symptoms with conservative management alone have usually engaged in MALS & Ehlers-Danlos Syndrome aware general physiotherapy, respiratory physiotherapy, osteopathy, exercise physiology or a combination of these (big shout out here to the Connected Health Alliance physical therapy team, based in Wollongong NSW).
Here is a blog post by a vascular surgeon which covers a few potentially relevant factors around posture, which I find interesting and anecdotally have had a few clients report improvement from (note: only implement change with supervision from your physical therapy team).
Good medical support from your GP, pain specialist or similar can also go a long way. There is still so much that the healthcare community is learning about these conditions.
Dietetic Management
How Dietitians assist clients with MALS will look very different for each individual. For some clients, dietetic therapy is able to help provide a significant reduction in symptoms, and for others, our goal is to avoid exacerbating symptoms while preventing further nutritional decline.
As Dietitians, here are some common areas we may assist our MALS clients with:
Managing malnutrition and gastrointestinal symptoms via food fortification, texture modification and adaptive oral strategies | tinkering with the texture (e.g. solid vs liquid) and composition of food can ease upper gastrointestinal symptoms for some MALS clients, while managing nutrition status. We can often suggest food fortification strategies here (e.g. ways to boost nutritional content of food) or prescribe hospital-grade oral nutrition supplements. If you notice signs of malnutrition increasing (see here for how Dietitians assess malnutrition in Australia - noting that an overall 'A' score means at risk of malnutrition, 'B' means moderate malnutrition and 'C' means severe malnutrition), chat to your healthcare team.
Postural changes | most people with MALS find that digestive symptoms can ease a bit in certain positions. We may explore variations on these to allow you to eat a bit more food, in a bit less discomfort.
Clear fecal loading | this is very common in hypermobile humans, and can significantly impact overall gut motility, inflammation (via mast cells and nervous system), microbiome and more.
Keep on top of dysautonomia and MCAS | this will support better autonomic nervous system function and inflammatory responses, which have many relevant impacts.
Make a malnutrition action plan | chat to key people in your health team - what steps are within reach to reduce malnutrition from worsening (if present) or occurring? When is it time to seek additional help, and where can you go? How can you adapt nutrition during these times? Noting that waitlists often take several months-years.
Interventional MALS Management
Coeliac Plexus Block
This is an emerging therapy (and diagnostic tool) for MALS, particularly individuals who have neurogenic compression. The block is usually performed by an interventional pain specialist, interventional radiologist or surgeon, and it is minimally invasive. For some people with MALS, coeliac plexus blocks provide significant relief for a few weeks, however for others, the relief may be mild and short-lived.
There is emerging research suggesting that people with MALS who respond well to coeliac plexus blocks may be better candidates for specific MALS surgeries, but more investigation is needed and there are currently very few surgeons in Australia who provide these surgeries.
Enteral and Parenteral Feeding
For clients whose MALS is significant enough to be severely limiting food and fluid intake, and causing malnutrition, enteral or parenteral nutrition may be discussed.
Interventional enteral nutrition for clients with significant MALS and malnutrition often takes the form of tube feeding (information about tube feeding pathways in Australia here) into the small intestine, via a nasojejunal (NJ) tube, or surgical jejunal ('J-tube') or gastro-jejunal ('G-J tube') tube. Feeding into the small intestine allows the food to bypass the stomach, where MALS usually impacts blood flow and motility.
Parenteral feeding is typically considered when tube feeding is not tolerated despite extensive troubleshooting. In the context of MALS, this may be necessary when individuals are severely affected by visceroptosis, which can exacerbate mesenteric ischaemia and lead to partial or complete intestinal failure. Parenteral feeding involves delivering broken down, liquid nutrition directly into the bloodstream, usually through a central like like a port or PICC.
Surgical Management
There are several surgeries that may help to manage or relieve symptoms associated with neurogenic and vascular MALS. Note that in Australia, very few surgeons offer these, with limited-to-no access via public healthcare. Other impacts associated with Ehlers Danlos Sydromes and hypermobility must be considered to ensure the surgery and recovery are successful (click here for Dr Jason Lam & Sharon Hennessey's Hypermobility Perioperative Guide).
Conclusion
In summary, I hope this has helped bring a bit more clarity around what MALS is, and potential management pathways. If you're currently navigating a MALS diagnosis or exploring the possibility, I'm sending you gentle virtual hugs. Health journeys - especially when living with hypermobility and vascular compressions - can be incredibly tough and frustrating. But with the right support, information and strategies, finding ease and clarity is absolutely possible.
~ Savvy
If you are looking for support with SMAS or other vascular compression syndrome like MALS, our team at Savvy Dietetics may be able to help. As a team, we are committed to providing high quantity & comprehensive dietetic care for hypermobile humans - involving ongoing education, and case conferencing with our both within our team weekly and externally with Australian colleagues.
Disclaimer: the information above is for education purposes only. Please consult with your medical and allied health team for personalised advice.
This blog was originally published on 8th September 2025, and received 480 views before we migrated websites in January 2026.
References:
https://acmdtt.com/wp-content/uploads/Ultrasound-Findings-in-Median-Arcuate-Ligament-Syndrome.pdf
https://vascsurg.me/2021/01/24/nonoperative-management-of-median-arcuate-ligament-syndrome-mals/
https://journals.lww.com/acgcr/fulltext/2021/10000/often_overlooked_diagnosis__median_arcuate.5.aspx
https://www.ucmals.com/diagnosing-mals-the-role-of-doppler-ultrasound-ct/